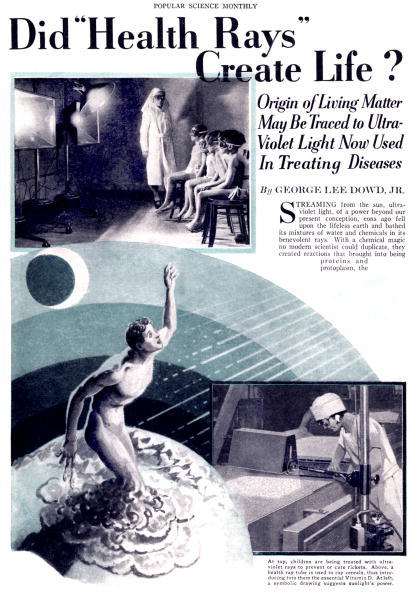
Light therapy was popular in Europe from the turn of the century until the late 1930s. The treatment had two branches: heliotherapy (natural sun therapy) and phototherapy (artificial light therapy). These progressive therapies presented and sold light as curative and transformative. The Sunray treatments were not only for the elite. Britons could buy their own units for the home (a big business in special lamps and devices grew), or pop into a hospital for a free dose of light – places like the Royal London Hospital, which opened a Light Department in 1899.

Health cure in the Institut Finsen, Copenhagen / Denmark, patients getting treatment with electric light, date unknown, probably around 1901
Wellcome Trust Research Fellow Dr Tania Woloshyn has researched light therapies:
Sunlight, whether natural or artificially-produced, could be used locally, that is directly onto wounds or lesions, or generally as a ‘bath’ for the whole body, and was understood to possess bactericidal and analgesic properties. As such light became a powerful, natural regenerative agent in the treatment of acute and chronic diseases.
…
At its zenith in the 1920s light therapy was widely accepted by the medical community and the public. And yet, I am discovering, it stood on shaky ground. Even then, reports in medical journals had begun to claim that ultraviolet light could cause skin cancer, and cases of overexposure – some fatal – led anxious physicians to cry out for regulation.
Measuring exposure became a major preoccupation in the drive to validate light therapy. Like other drugs, sunlight needed to be dosed in the right quantities to do good rather than harm. But regulating and monitoring ‘correct’ exposures for each individual, whether the sick patient or the sun-lover on holiday, have proved to be elusive goals, as much for practitioners then as is the case now for the NHS and cancer charities.
Today’s contradictory attitudes towards the sun’s rays are not new; they have existed since light therapy’s inception during the 1890s. The question ‘Is sunlight good or bad for us?’ has no simple answer – and consequently it has a truly fascinating history.

circa 1900: A woman inspects an Electric Bath at the Light Care Institute. The Electric Bath is probably a forerunner of the modern sunbed, although it was more likely used for medicinal reasons. (Photo by Reinhold Thiele/Thiele/Getty Images)

circa 1900: A woman inside an Electric Bath at the Light Care Institute. The Electric Bath is probably a forerunner of the modern sunbed, although it was more likely used for medicinal reasons. (Photo by Reinhold Thiele/Thiele/Getty Images)
Healing Tools has a history of light therapy:
During the 1890s, ultra-violet was discovered to have a powerful anti-bacterial action. In 1903 a Dane, Neils Finsen, was awarded the Nobel Prize for his work in treating skin tuberculosis with ultra-violet light. In 1920 Dinshah Ghadiali, an Indian, developed the Spectro-Chrome system of healing, after 23 years of exhaustive scientific evaluation. This was based on the relationship between colors and specific areas of the body. One of his most vocal supporters was the Chief Surgeon at Philadelphia Woman’s Hospital, Dr Kate Baldwin. She used Dinshah’s methods for many years and is quoted as saying “…after nearly 37 years of active hospital and private practice in medicine and surgery, I can produce quicker and more accurate results with colors than with any or all other methods combined – and with less strain on the patient…”.
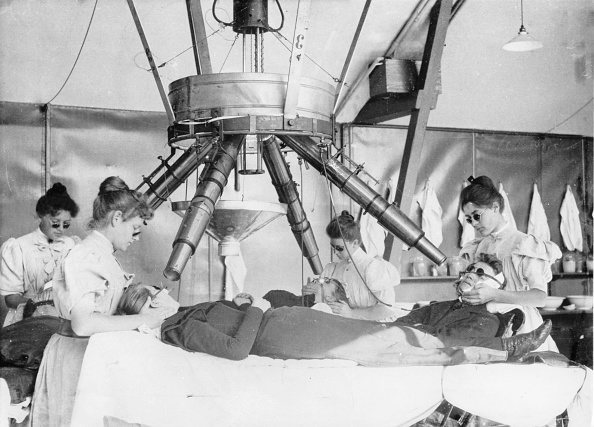
(GERMANY OUT) health cure in the Institut Finsen, Copenhagen / Denmark, patients getting treatment with electric light, date unknown, probably around 1901 (Photo by ullstein bild/ullstein bild via Getty Images)
While Dinshah was focusing on applying light directly to the body, Harry Riley Spitler was looking at treating the body by way of the eyes. During the 1920s and 1930s he developed the principles of syntonics (from the word ‘syntony’ – to bring into balance) in which light is used to balance the sympathetic and parasympathetic nervous systems. His College of Syntonic Optometry is now at the forefront of developments in ocular phototherapy. Spitler is generally considered to be the father of colored light phototherapy.
Sun therapy (heliotherapy) was very popular in Europe from around the turn of the century until the late 1930s. One of its foremost practitioners was Dr Auguste Rollier who established a sun-therapy clinic in Leysin in the Swiss Alps. He treated all sorts of patients, very effectively, particularly those with TB – his patients would be wheeled out onto a large sundeck for specific periods each day.
In the 1930s, Charing Cross Hospital in London used ‘sun-lamps’ to treat circulatory diseases, anaemia, varicose veins, heart disease and degenerative disorders. Then in the early 1940s in the USA, Emmitt Knott developed a very interesting device – a haemoirradiation machine. He went a stage further than Dinshah and Spitler and administered light to the whole body by irradiating just a small volume of blood.
Knott found that irradiation of just 50±100cc of blood with ultra-violet light and retransfusion back into the patient had a dramatic impact in the treatment of puerperal sepsis, peritonitis, encephalitis, polio and herpes simplex. By 1947, somewhere in the region of 80 000 patients had been treated with reported success rates of 50-80%.
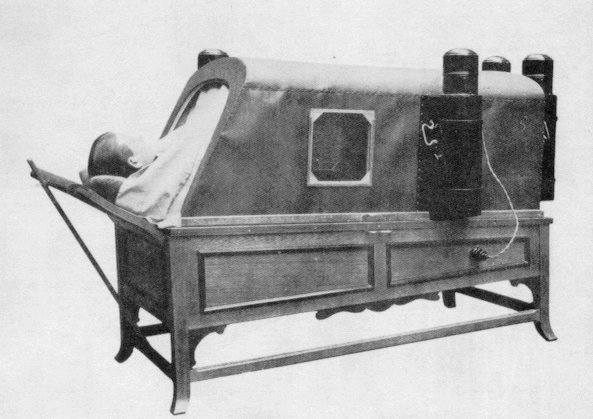
Electric Bath as used on The Titanic (1912) Via

February 1921: Patients receiving treatment in the Electrical Department of St George’s Hospital, Hyde Park Corner, London. (Photo by A. R. Coster/Topical Press Agency/Getty Images)
The treatment was also available to children. Be prepared to see some creepy photos.

A child receiving treatment under an artificial sun lamp. (Photo by Topical Press Agency/Getty Images)
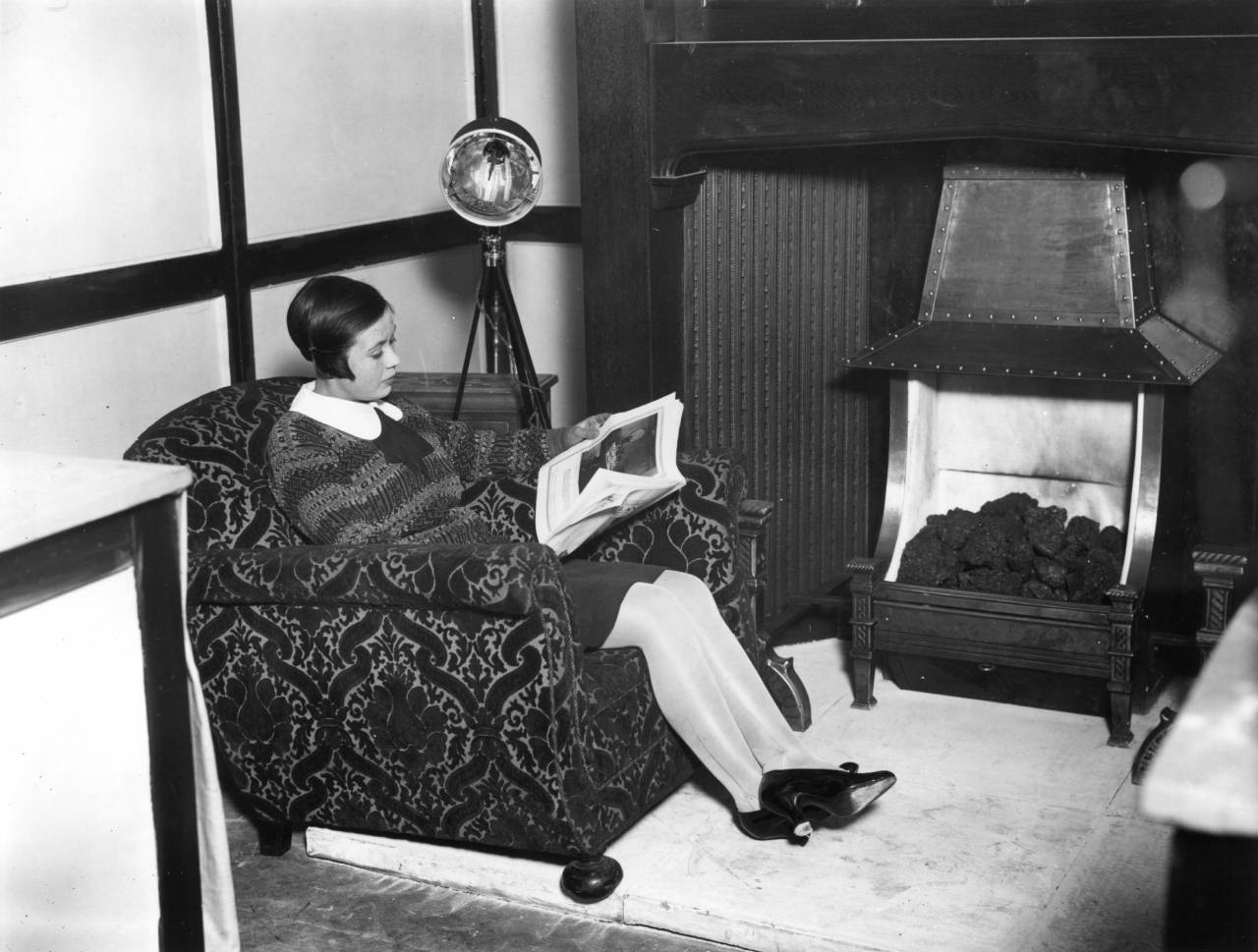
circa 1927: A woman under a sunray lamp, on show at the first International Exhibition of Light and Heat in Medicine at Central hall, Westminster. (Photo by Topical Press Agency/Getty Images)
Nobel Laureate Niels Ryberg Finsen was at the forefront of the light as medicine movement. The aforementioned Royal London used his eponymous Finsen Lamp. He wrote:
I suffered from anaemia and tiredness, and since I lived in a house facing the north, I began to believe that I might be helped if I received more sun. I therefore spent as much time as possible in its rays. As an enthusiastic medical man I was of course interested to know what benefit the sun really gave. I considered it from the physiological point of view but got no answer. I drew the conclusion that I was right and the physiology wrong. From this time (about 1888) I collected all possible observations about animals seeking the sun, and my conviction that the sun had a useful and important effect on the organism (especially the blood?) became stronger and stronger. What this useful effect really was, I could not find; I have been working for this goal ever since but have not been able to find exactly what I have been seeking, though we have gone somewhat forward.
My intention was even then (about 15 years ago) to use the beneficial effects of the sun in the form of sun bathing or artificial light baths; but I understood that it would be inappropriate to bring it into practical use if the theory was not built upon scientific investigations and definite facts.
During my work towards this goal I encountered several effects of light. I then devised the treatment of small-pox in red light (1893) and further the treatment of lupus (1895). Both these things are therefore in a sense side-issues, but they completely occupied my time for several years and have partly drawn me away from my main goal.
During the last few years, I have, however, become convinced that it does not help to wait until I find the answer I am looking for in the laboratory, but that it is justified to work also with clinical experiments. Thus both approaches can be carried out simultaneously in the effort to reach the final goal.

circa 1925: American comedienne Florence Mills basks in the glow of a sun lamp in her dressing room. (Photo by General Photographic Agency/Getty Images)
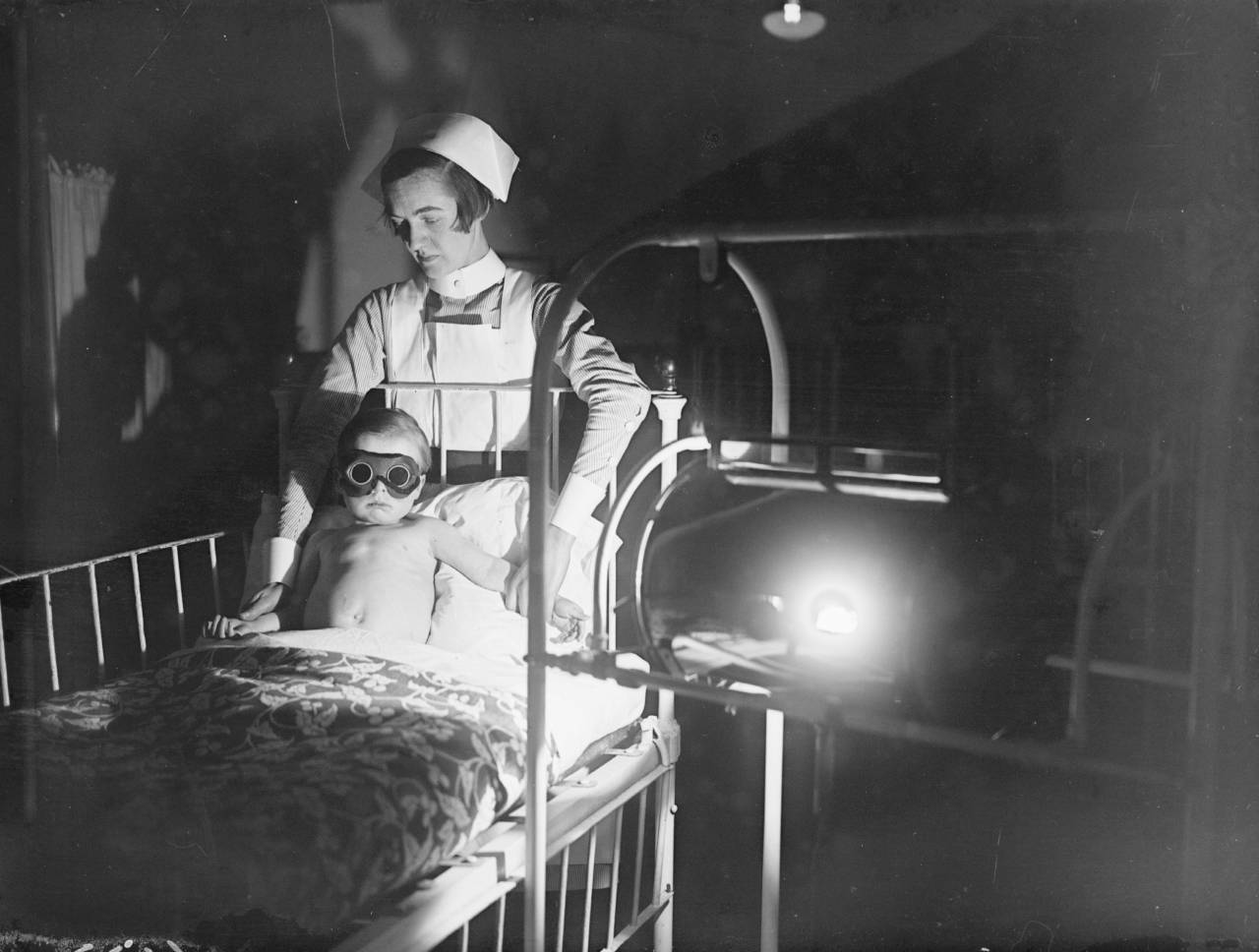
February 1928: A child wearing goggles and held by a nurse, undergoes sun-ray treatment at Cheyne Hospital for Children, Chelsea. (Photo by Fox Photos/Getty Images)

circa 1929: 23 year old Alma Smith, the ‘cleverest soubrette’ of the cast of ‘Blackbirds’ at the London Pavilion, receiving her daily dose of ultra violet rays from a sun machine.
Did it work? Was it all quackery? The James Lind Library highlights the work of Dora Colebrook (1884-1965). She took the trouble to investigate the booming light therapy business. Martin Edwards tells the story:
Colebrook owed her introduction to the Medical Research Council (MRC) to her brother, the respected bacteriologist Leonard Colebrook. The MRC, which was afraid of being overtaken by the rapid expansion in light therapy before the Council could adjudicate on its effectiveness, established a Clinical and Biological Sub-Committee to the Committee on the Biological Actions of Light and appointed Colebrook to act as its secretary.
Colebrook chose to study two areas where light therapy was almost universally believed to be beneficial: the treatment of varicose ulcers, and of ‘weedy’ or ‘sickly’ children. In 1927 she treated 84 patients with varicose ulcers, comparing conventional treatment with paste and dressings against light therapy. Eleven large ulcers were partially treated, half the ulcer being exposed to light while the other half was shielded as a control, a method of testing that had been used to assess treatments for burns five centuries previously (Paré 1575). Colebrook was unable to detect any beneficial effects of light therapy on varicose ulcers; indeed, paste dressings fared rather better than treatment with light (Colebrook 1928).
Colebroook conducted her schoolchildren study in a Willesden Council infant school, allocating 287 children into one of three groups – to receive no therapy, light therapy from an arc device, or therapy from an arc device shielded by glass to exclude the ultraviolet component (there was considerable debate, at the time, as to the relative therapeutic merits of visible and ultraviolet light)… Although Colebrook sought consent from parents for the involvement of their children in the study, she did not inform them that two types of light therapy were going to be compared. Her study was single blind (she and her co-investigators were aware of which children received which type of light)…
Once again, she was unable to show any beneficial effects of light therapy: no improvement was demonstrated in height, weight, incidence and duration of colds and other minor infections, school absence, school progress or overall wellbeing.
Her work was not universally well received.
Opposition to Colebrook’s findings was rapid, widespread, and frequently vitriolic. Many objected that Colebrook’s ‘scientific’ method was no match for the accumulated experience and wisdom of eminent physicians. A BMJ editorial (1929) preferred the insights of ‘a large body of experienced clinicians’ and a Lancet editorial (1929) opined similarly that so widely established a therapy must have therapeutic benefit, and that ‘in the long run, neither medical men nor the public can be deceived.’ Many practitioners wrote to express similar sentiments in these and other journals. The newspapers also became involved, the Times (1929) and Guardian (1929) carrying critical editorials and letters, and the Telegraph (1929) devoting an entire edition to the theme, with an editorial concluding that the long and distinguished pedigree of light therapy proved its value.
…
In 1946, Colebrook extended her light therapy research to study its effects among office and factory workers, and coalminers (Colebrook 1946)… Once again, Colebrook was unable to detect any benefits of light therapy. This time, medical responses to the results of her research were far less critical, although light therapy equipment manufacturers were vocal in their opposition. By the 1950s, the equipment manufacturers were fighting a rearguard action to preserve their claims for therapeutic efficacy against increasingly sceptical medical and public opinion.
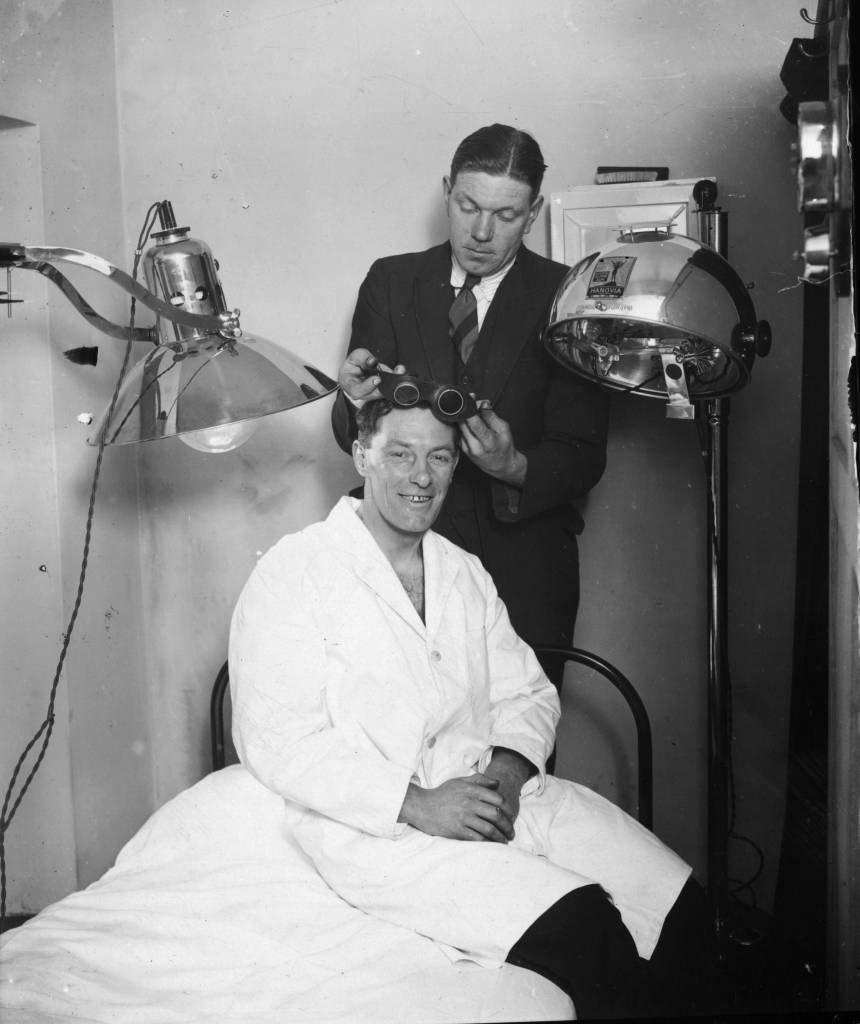
7th February 1929: Northampton Town Football Club trainer fits the team captain, W Watson, with some goggles for a course of ultra-violet ray treatment in preparation for an FA Cup tie with Millwall.

circa 1930: Hollywood film star, Dorothy Sebastian (1903 – 1957) undergoing treatment for bronchial congestion with a sun-ray lamp at MGM studios. (Photo by General Photographic Agency/Getty Images)

11th May 1931: Stripped to the waist and wearing goggles, children sit round a lamp having sun ray treatment while they listen to the gramophone at the East End Mission in Commercial Rd, London. (Photo by Fox Photos/Getty Images)

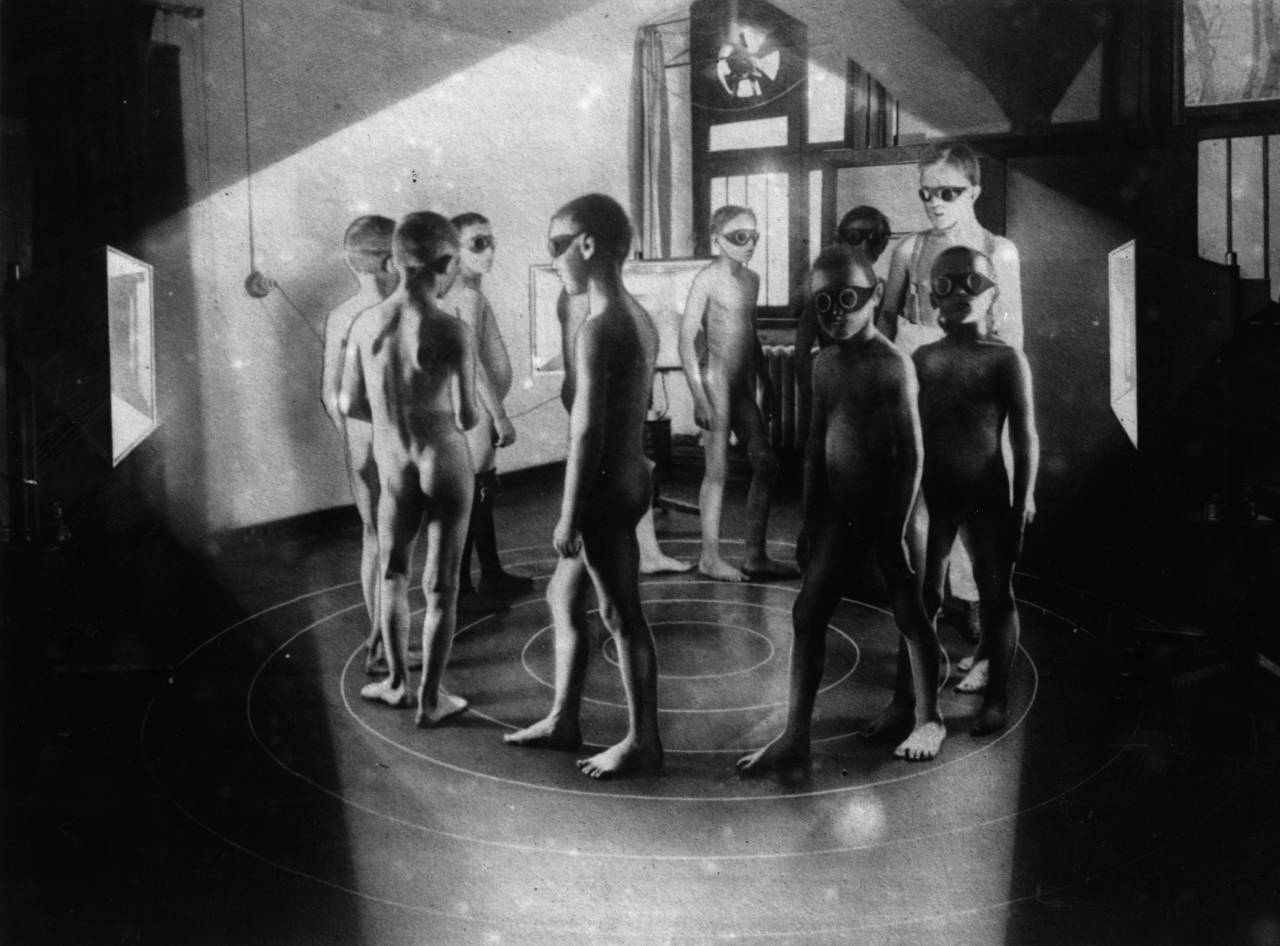
A group of children hold hands around a radiating glow of ultraviolet light at the Institute of Ray Therapy.

31st March 1930: A group of ladies relax on the sandy floor in the solarium of the Tolland Hotel, Bournemouth. (Photo by Fox Photos/Getty Images)

9th September 1932: A tall arched window letting in rays of sunshine into the drawing room of the eighteenth century house owned by Sir Wyndham Portal.
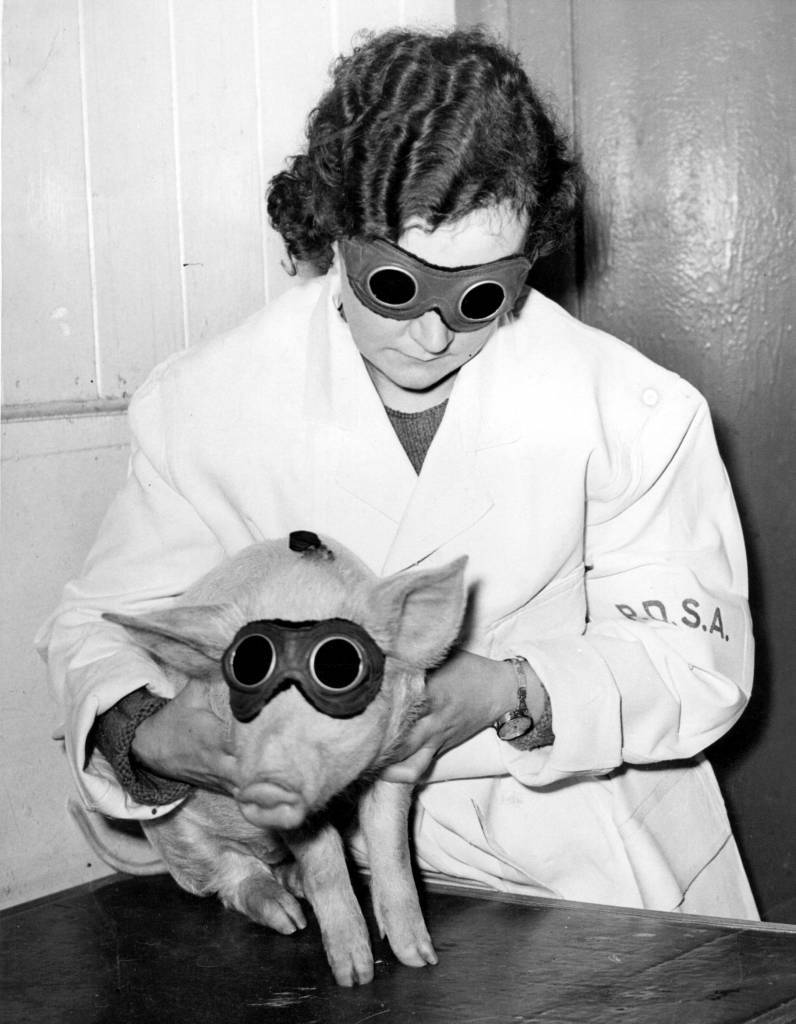
10th January 1938: A piglet which is being treated by the PDSA (People’s Dispensary for Animals) in Ilford with a sun ray lamp, to cure a skin ailment. (Photo by Fox Photos/Getty Images)
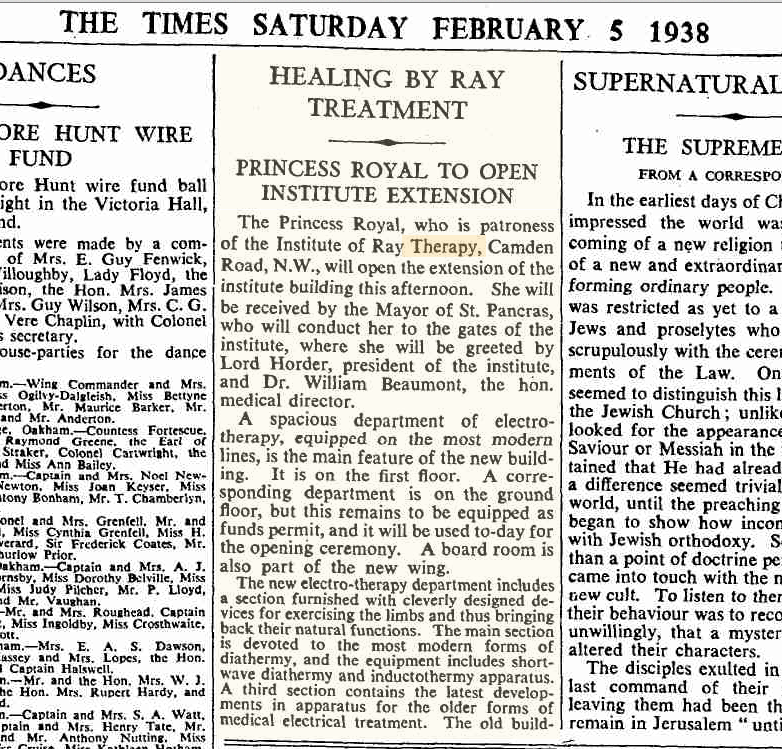
The Times, February 5, 1938:
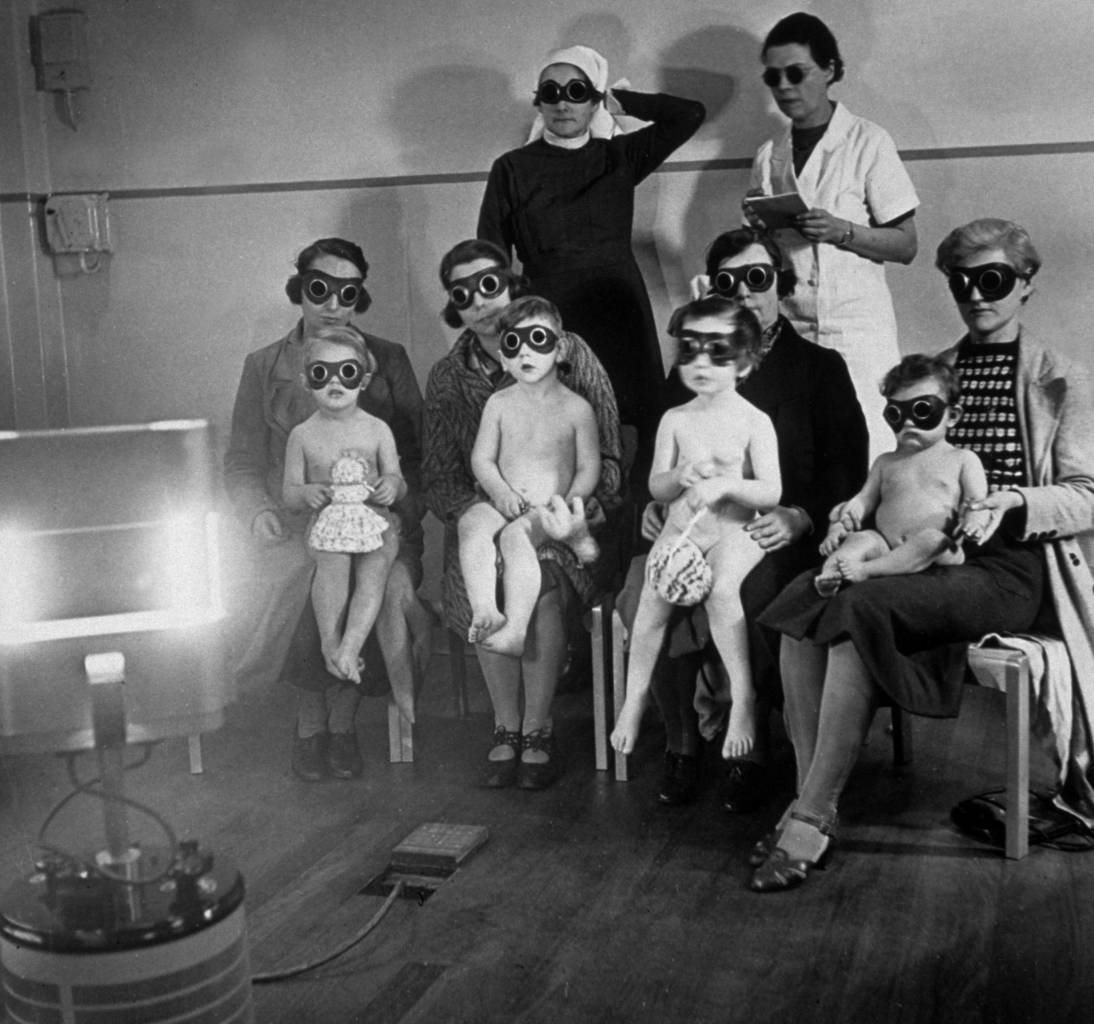
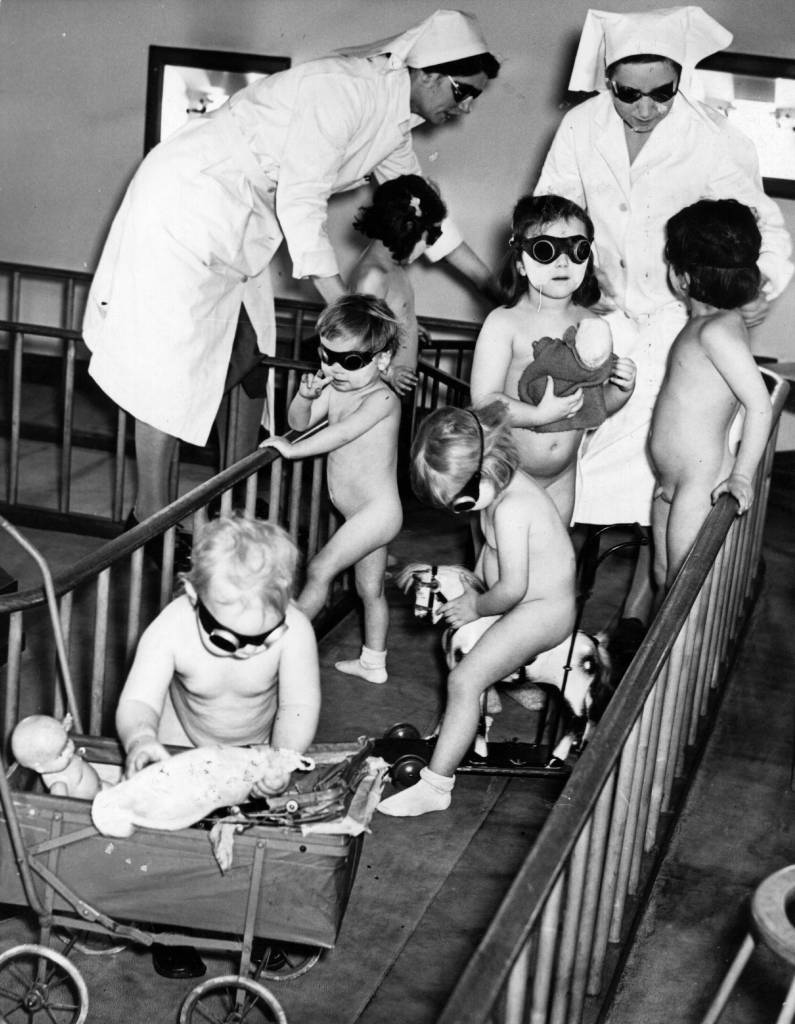
circa 1938: Children receiving ray treatment at the child welfare centre in Harrow Road, west London. (Photo by Hulton Archive/Getty Images)

January 1938: Three nurses and a group of young children sitting around a Centrosol sunray lamp at the Miriam Price Coleman day nursery. (Photo by Fox Photos/Getty Images)
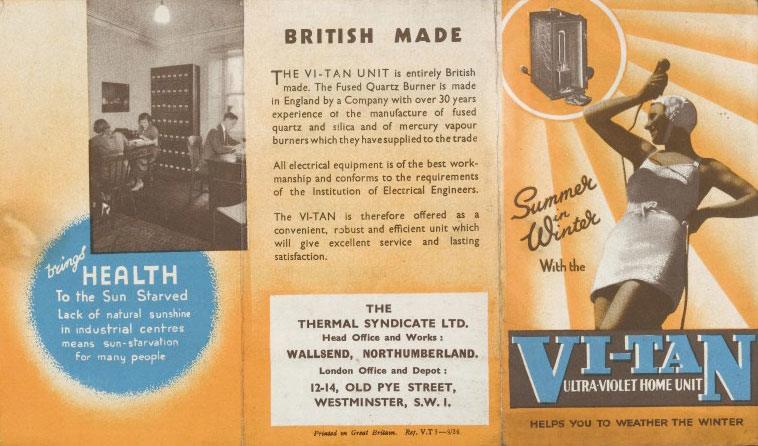
In a 1936 leaflet, a ‘Vi-Tan’ UV-rich mercury vapour lamp shines down on a jubilant woman. She is dressed for the beach but wrapped in an electrical cord. The manufacturers of the device, the Thermal Syndicate Ltd, promise that their UV lamp would bring “summer in winter” to the “sun starved, restoring everyone to a healthy colour”. Like the woman’s smiling face and her swimsuit body displaying delectable contours, the promise was that everyone could have a deeply tanned body. Through an overtly contrived composition, the Vi-Tan acted as the technologically advanced substitute for a radiant and radiating sun. The lamp was thus stationed in the advertising as though taking its ‘natural’ place, embedded within the sun itself.

16th March 1939: Children undergoing sunray treatment at Manchester’s Open Air School for Delicate Children. (Photo by Fox Photos/Getty Images)

13th December 1940: Two crew members of a British submarine spend a session under a sunlamp whilst ashore, to make up for the time they spend below the surface without being subjected to sunlight. (Photo by Arthur Tanner/Fox Photos/Getty Images)

A physical therapist supervises a young polio sufferer’s ultraviolet treatment, while protective glasses shield his eyes from the potentially harmful rays. (Photo by Vecchio/Getty Images)

24th May 1941: An RAF Flying Officer receiving Sun-Ray and electrical treatment after suffering a broken back. (Photo by P. R. Poukev/Fox Photos/Getty Images)
1942: All officers at the RAF fighter headquarters who work underground are provided with sun ray treatment from a lamp presented by Lord Nuffield. (Photo by Keystone/Getty Images)

2nd March 1942: A nurse watching over children in Bermondsey, London, sitting under sun-ray lamps to help make up the deficiency in sunlight and the lack of certain items of food, such as fruit, during the winter months of the Second World War. (Photo by Fox Photos/Getty Images)
2nd March 1942: Children from Bermondsey London playing in artificial sunlight in a solarium with a sunlamp providing the ‘sunshine’.
circa 1943: Children receiving ultra-violet treatment during World War II. (Photo by General Photographic Agency/Getty Images)

17th April 1942: Civil Defence Workers in Finsbury are beating the winter pallor with free sun lamp treatments. They call it ‘Mixray’ at the Finsbury Health Centre, and it was designed by two Czechoslovak inventors. (Photo by Harry Todd/Fox Photos/Getty Images)

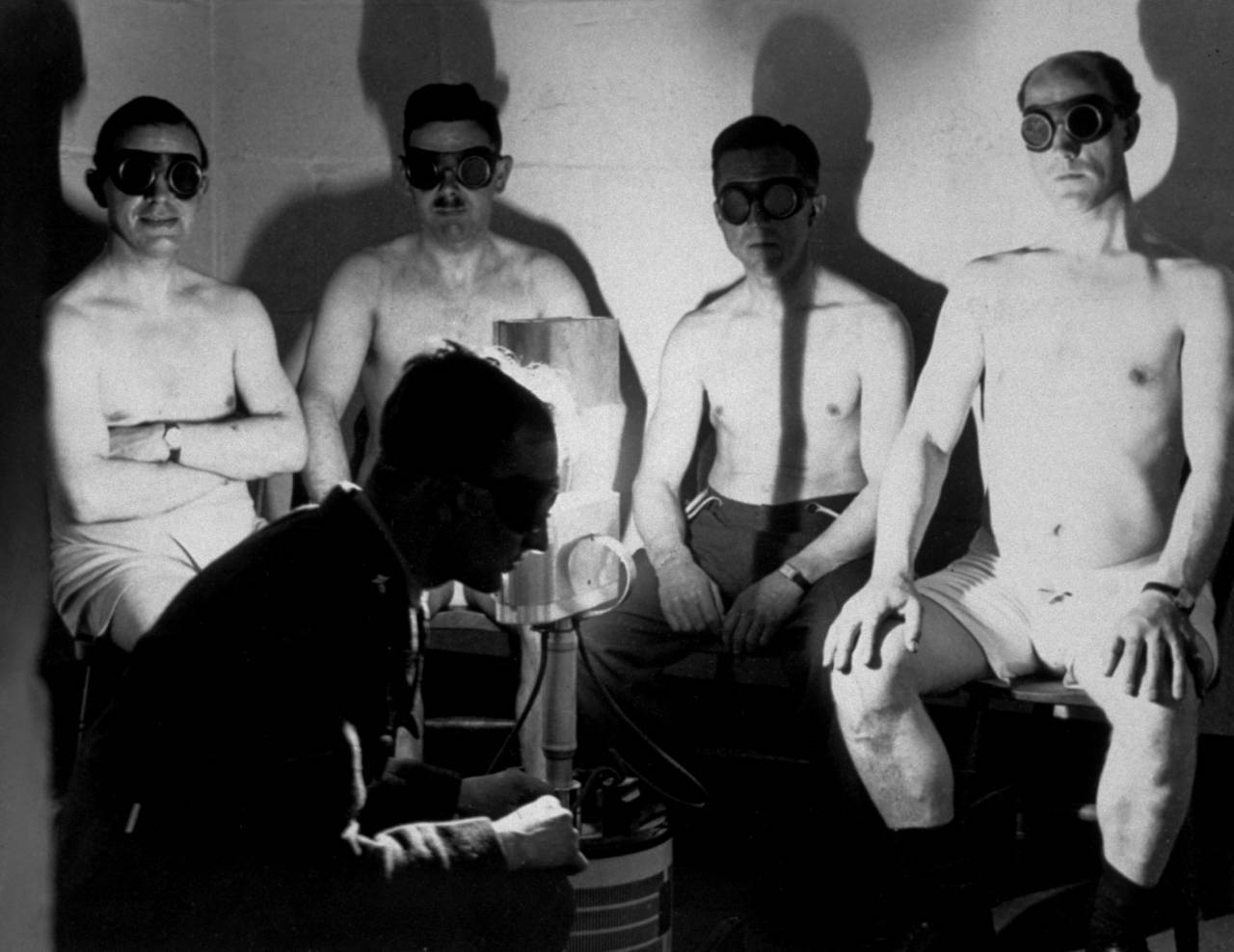
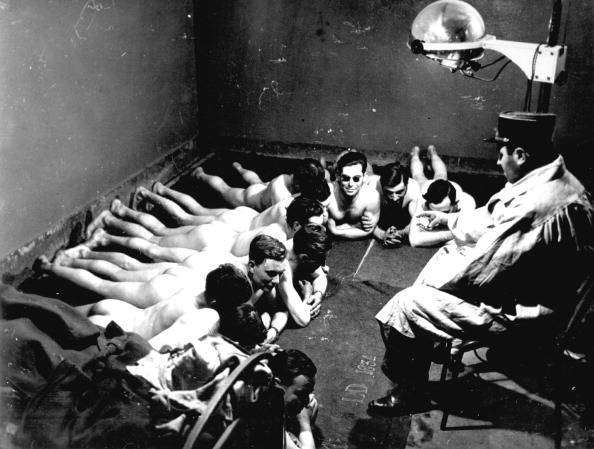
(GERMANY OUT) Nude miners are waiting for admission to the irradiation room (solarium) – Photographer: Werner Cohnitz, Dietrich Kenneweg- Published by: ‘Berliner Illustrirte Zeitung’ 03/1940Vintage property of ullstein bild (Photo by Werner Cohnitz/ullstein bild via Getty Images)

Under the guidance of a qualified Therapist miners receive a dose of ultra violet and infra red rays from special lamps set up in this solarium, 16th December 1947
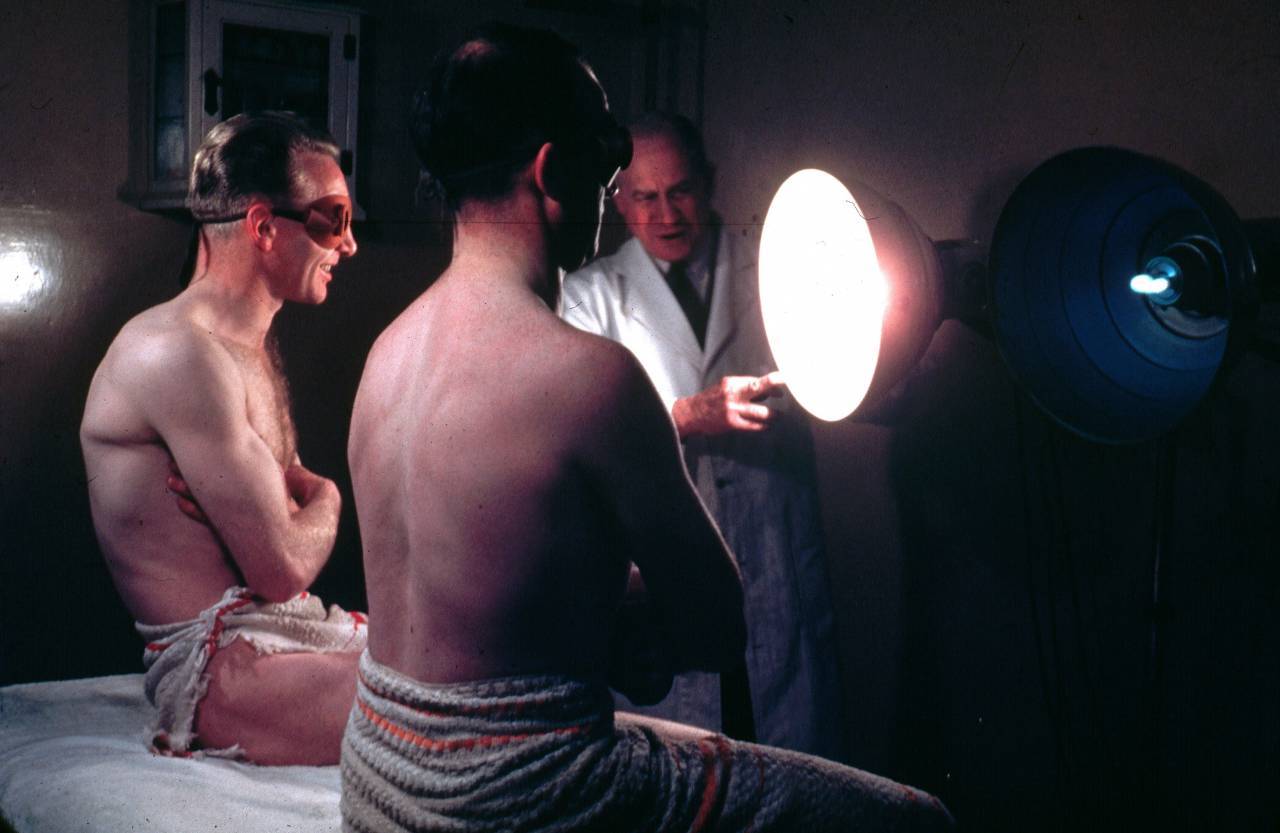
circa 1950: Two men wearing protective eye goggles and towels sitting under sunlamps set up by a doctor. (Photo by Hulton Archive/Getty Images)
Would you like to support Flashbak?
Please consider making a donation to our site. We don't want to rely on ads to bring you the best of visual culture. You can also support us by signing up to our Mailing List. And you can also follow us on Facebook, Instagram and Twitter. For great art and culture delivered to your door, visit our shop.






![UNITED KINGDOM - JANUARY 01: Ultraviolet radiation of sick children, standing in a circle around the radiation apparat with their nurses. At the Institute for Radiation Therapy in London. 1934. (Photo by Imagno/Getty Images) [Ultraviolett-Bestrahlung von kranken Kindern, die mit Krankenschwestern im Kreis um das Bestrahlungsgeraet stehen, im Institut fuer Strahlentherapie in London. Photographie. 1934]](https://flashbak.com/wp-content/uploads/2015/09/56460898.jpg)

